It’s hard to ignore a toothache, and even if you can, it’s not always a good idea. Sensitivity or pain in the mouth is usually a sign that there is a problem. It might go away, but if it doesn’t, it could be a dental abscess.
A dental abscess is a bacterial infection at the root of a tooth. If a patient has one, they should see a dentist as soon as possible. If an abscessed tooth is left untreated, there is a risk that the infection will spread to other teeth or the jaw. It can also cause excruciating pain that will interfere with the patient’s daily life.
Dental Abscess Symptoms to Watch For

The primary symptom of an abscess is constant, throbbing pain. It will hurt to bite down and there might also be sensitivity to hot, cold, or sweet things.
An abscess differs from other tooth ailments. It causes pus to gather in a pocket around the area. This results in a swollen fluid-filled “bubble” on the gums near the infected tooth. This bump or bubble might be red and look inflamed, and will add to the feeling of pressure and discomfort in the tooth itself.
If a patient has what they think might be an abscess, they should make an appointment to see the dentist. The dentist will be able to tell exactly what it is and how to treat it. If the condition progresses to include fever or the swelling spreads to the face, neck, or lymph nodes under the jaw, the situation is more urgent and the dentist should be seen immediately. If a fever gets very high or swelling makes it hard to breathe or swallow, go to an emergency room right away.
What Causes an Abscess
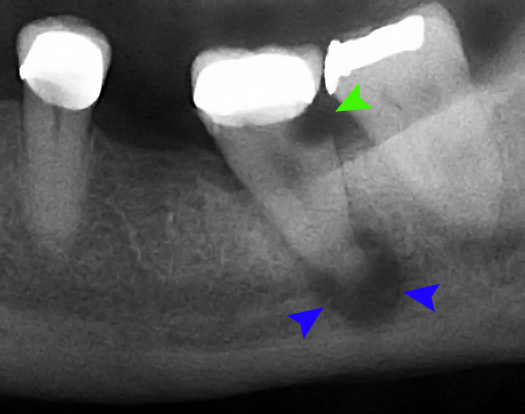
The Mayo Clinic defines an abscess as “a pocket of pus that’s caused by a bacterial infection.” There are three types of abscess: periapical, periodontal, and gingival.
A periapical abscess is an infection in the root of a tooth at the tip. This is the type of abscess covered in this article.
Periodontal abscesses are infections of the gums caused by gum disease.
Gingival abscesses happen when a foreign object gets stuck in the gum and causes an infection.
An abscessed tooth occurs when bacteria gets down into the root of the tooth, infecting the soft tissue there. At the core of the tooth is a bundle of nerves and blood vessels that carry nutrients from the gums up into the tooth. The bacteria usually get in through a cavity, or a crack or break in the tooth. Cavities start out as just a tiny pit in the tooth’s surface, but if they are not filled, they will grow bigger and deeper over time until they reach the center. A break in the tooth can expose the root to bacteria right away.
Once the bacteria is in the root, it will attack the tissue there, making it swell. The inflammation has nowhere to go, so the pressure builds up and makes it painful. This is a condition called pulpitis. Eventually, the surrounding gum tissue will fill with bacterial fluid, or pus, that has seeped out of the root, and an abscess forms.
Treating a Dental Abscess

Until they can seek treatment, patients can find some relief with over-the-counter pain relievers and topical analgesics. They may also try rinsing their mouth with warm salt water or applying cold compresses to their jaw. These will not fix the problem but can help with the pain until they get to a dentist.
A dental abscess is considered a dental emergency. Once a dentist determines there is an abscess, they will quickly make arrangements to treat it. The first step will be to drain the pus that has collected. This is something that a patient should never try to do themselves.
Sometimes, an abscess will burst and drain on its own. If that happens, the patient should still see the dentist anyway. The infection is still there and the tooth must still be fixed.
When tooth decay has made its way all the way to the root of a tooth, and the bacteria has been extensive enough to cause an abscess, a root canal procedure is almost certainly necessary. A root canal involves the dentist or an endodontist drilling into the tooth, removing the infected tissue, and filling the hole. A dental crown is usually placed over the tooth to seal it from further decay.
In very severe abscess cases, the tooth may not be able to be saved and extraction may be recommended.
When the procedure is done, the dentist may prescribe antibiotics to kill any infection that remains. The tooth should be back to normal and pain-free after a few days.
Left untreated, abscesses will not go away. The pain will continue and possibly get worse. The infection can spread further into surrounding teeth, gums, and jaw. Bone loss can occur. It can be difficult to swallow or breathe. In the worst cases, sepsis can set in. Sepsis is a potentially life-threatening condition where an infection moves through the bloodstream throughout the body.
Is it an Abscess or Something Else?
Having pain in the mouth or sensitivity does not always mean there is an abscess. Without that telltale symptom of pus, there are several other possible dental issues that could be causing a patient’s discomfort.
Something as simple as a small seed or other food particle stuck between teeth can be surprisingly painful and make it difficult to eat. Brushing and flossing around the tooth can sometimes dislodge whatever is stuck.
If a patient grinds his or her teeth (called bruxism), or if their wisdom teeth are coming in, their teeth and jaw may be sore and sensitive. Both can cause some pain but are easily remedied. Bruxism can often be corrected with the use of a mouthguard. Wisdom teeth usually have to be removed.
Pain will result from a tooth, filling, or dental crown breaking or cracking. If the pain doesn’t go away after a while, a dentist should be contacted to repair any damaged teeth. The pain might not indicate an abscess, but the crack in the tooth could let bacteria in to start one.
Gum disease can be painful too and can lead to a periodontal abscess. This is an infection of the gum near a tooth’s root, rather than a periapical abscess that is in the tooth itself. Treatment for a gum abscess is different than that for a tooth abscess and is performed by a periodontist instead of a dentist or endodontist.
Some things will cause pressure or sensitivity even when teeth are healthy. Sinus problems can make the top teeth sore as the sinuses swell. And overuse of teeth whitening products can make teeth sensitive. Luckily, neither condition is usually painful enough to be mistaken for an abscess and should subside after a while.
Know How to Spot an Abscess
The pain from an abscess is usually described as severe and persistent. It will radiate out from the area of the affected tooth. The gum nearby might be red and swollen with the blister-like pocket of pus. With all of these symptoms at once, a patient can be fairly confident that they have an abscess. Dental abscesses are much more than just a toothache and should be taken seriously, with a dental visit and treatment. If you don’t have a dentist, you can find one using our online search tool.


